This clinical case highlights an uncommon dermatological condition with systemic involvement that deserves consideration in primary care. The patient is a 55-year-old woman with a medical history of hypertension and chronic obstructive pulmonary disease (COPD). She had no known allergies, smoked around ten cigarettes daily, and had been taking enalapril for six years along with inhaled formoterol for two years. As her respiratory condition worsened, her pulmonologist decided to modify her treatment, discontinuing formoterol and initiating a new inhalation therapy combining indacaterol and glycopyrronium in capsule form.

Two days after starting the new inhaler, she visited her primary care provider complaining of painful red patches on her cheeks and neck, accompanied by a low-grade fever. She denied any recent changes in her skincare routine or diet and reported no upper respiratory symptoms, although she did mention recent sun exposure with proper protection. Given the appearance of the lesions and associated systemic symptoms, she was urgently referred to the dermatology department for further evaluation. The dermatologists recommended discontinuing the new inhaler and conducted a skin biopsy along with laboratory tests including a complete blood count, autoimmune markers, lupus anticoagulant, and serologies.
She was prescribed oral corticosteroids. Within 24 to 48 hours of starting corticosteroid treatment, the painful lesions began to fade, and her discomfort decreased significantly. Blood work revealed leukocytosis with a predominance of neutrophils, while antibody tests, lupus anticoagulant, and serologies were negative. About twenty days later, the biopsy results confirmed the diagnosis of Sweet syndrome, also known as acute febrile neutrophilic dermatosis. This rare inflammatory condition falls under the group of neutrophilic dermatoses and is histologically identified by dense infiltrates of neutrophils in the skin.
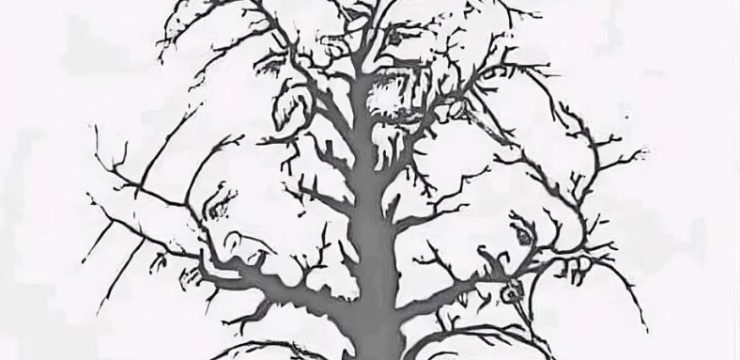
Clinically, Sweet syndrome presents with the sudden appearance of painful, erythematous papules or plaques, typically distributed asymmetrically on the face, neck, upper trunk, and hands. It is frequently associated with systemic symptoms such as fever and elevated white blood cell counts, specifically neutrophilia. The exact cause of Sweet syndrome remains unclear, but current research suggests that cytokine-mediated pathways play a key role in recruiting and activating neutrophils and histiocytes. It is often considered a hypersensitivity reaction, potentially triggered by upper respiratory infections, underlying cancers, autoimmune diseases, or exposure to certain medications. In drug-induced or idiopathic cases, the condition is more common in women.
A wide variety of drugs have been associated with Sweet syndrome, including contraceptives, antiepileptics, antibiotics, antihypertensives, colony-stimulating factors, and vaccines. However, this case is notable because the syndrome followed the use of an inhaled medication—specifically a combination of indacaterol and glycopyrronium—which has not been previously linked to Sweet syndrome in the literature. This suggests the need to consider less commonly implicated drugs as potential triggers, especially when a clear temporal relationship exists between drug initiation and symptom onset. Treatment with oral corticosteroids is typically very effective, often resulting in rapid relief of symptoms and resolution of skin lesions within a week. In cases like this, where the presentation includes erythematous papules and plaques on the face and neck, it is crucial to differentiate between Sweet syndrome and other conditions such as urticaria, contact dermatitis, drug-induced toxicoderma, and cutaneous lupus. Accurate diagnosis depends on thorough clinical evaluation, laboratory testing, and, importantly, skin biopsy. Although Sweet syndrome is rare and often not considered early in the diagnostic process, it should be kept in mind due to its potential systemic involvement and associations with infections, autoimmune diseases, and malignancies, particularly hematologic cancers. Once the diagnosis is made, further investigation is essential to rule out associated conditions such as neoplasms, rheumatic diseases, or hidden infections. For primary care physicians, maintaining a broad differential diagnosis is essential, even when the precise diagnosis isn’t immediately clear. Awareness of rare diseases like Sweet syndrome can lead to earlier referrals and more effective treatment, improving patient outcomes. This case serves as a reminder of the need for vigilance in evaluating new symptoms following medication changes and the importance of considering rare diagnoses when common ones have been excluded.